From the moment COVID-19 locked down the world, we were all hoping for a treatment or vaccine to aid in our fight against the coronavirus, sooner rather than later.
Fast forward, today mRNA vaccines have played a major role in our ability to return to almost pre-pandemic normality. Considering the speed at which it was developed, alongside the impact it has had on humanity’s fight against COVID-19, what does the future hold for this technology as humanity presses on to near normal living?
What is an mRNA vaccine?
To answer this question, let’s take a trip back to our high school biology class to first understand what mRNA is. Messenger Ribonucleic Acid (mRNA) is naturally found in our bodies. It is a molecule that helps the cells in our bodies convert genetic material into proteins. Essentially, mRNA are molecules that carry a ‘copy’ of specific instructions from our DNA to our cells in order for them to create proteins.
As explained by Dr Husna Musa, “Imagine if your local library had a recipe book that contained recipes for all Malaysian dishes. That recipe book is our DNA. Now, let’s say that you’re interested in creating one particular recipe from this book. This recipe refers to the specific genetic material. In this case, mRNA would be similar to making a photocopy of that recipe, which you can then take home to create the dish or the protein.”
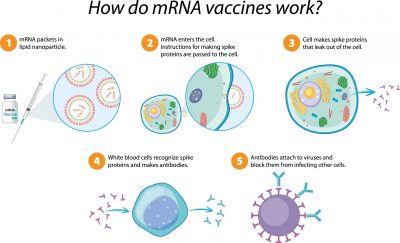
Knowing how mRNA works is essential to understanding how it can be used in a vaccine. “mRNA vaccines contain mRNA molecules with the instructions to create a piece of a pathogen (antigen) which would induce the formation of protective antibodies. Upon injection into the body, the cells can then take these instructions and create the antigen (in the case of SARS-CoV-2, it is the spike protein). The antigen would stimulate the immune system to produce antibodies without actually being infected by the pathogen. Therefore, mRNA vaccines are like delivering the photocopied recipe (mRNA) to an individual so that they can make the dish or the protein themselves,” the paediatrician explains further.
COVID-19 mRNA vaccines: Effectiveness, concerns, and side effects
With the ever-growing sea of information that is available online, it is difficult for parents to find a straightforward answer about COVID-19 mRNA vaccines. More often than not, they are left drowning in pages of clinical trial data sheets and research papers filled with scientific jargon. It is therefore extremely important for parents to be able to receive accurate, factually correct, and simplified information in order to make their own informed health decisions for themselves and their families.
As mentioned by Dato Dr Musa Mohd Nordin, “Speaking on the effectiveness of COVID-19 vaccines as a whole is not as easy as providing a simple ‘Yes’ or ‘No’. There are many factors that need to be considered when discussing the effectiveness of a vaccine. For example, how effectiveness is being measured? Which age groups are we talking about? And against which strains of COVID-19?”
The consultant paediatrician explains, “Generally speaking, the COVID-19 mRNA vaccines available in Malaysia are highly effective at preventing severe COVID-19, hospitalisation and death. A recent local study found that being fully vaccinated against COVID-19 with an mRNA vaccine had up to 92.5% and 96.5% vaccine effectiveness in preventing ICU admission and preventing death due to COVID-19 respectively. The risk of dying from COVID-19 in an unvaccinated person is 14.3 times higher compared to a person who has received 4 doses of the vaccine.”
The effectiveness of a particular vaccine is one of many aspects to consider before committing to get the jab. However, safety is also another important factor to consider. “Many have concerns about the side effects of the COVID-19 mRNA vaccines, and rightfully so. However, studies have shown that COVID-19 mRNA vaccines have an acceptable safety profile, with the majority of patients experiencing common side effects that are usually temporary and mild, such as pain at the site of injection, chills, fatigue, fever, headache, nausea, and diarrhoea,” he adds.
In regards to severe side effects, Dato Dr Musa explains, “Severe side effects are rare. The National Pharmaceutical Regulatory Agency (NPRA) reported 26 serious cases per 1,000,000 doses. However, the majority of these serious cases only required close observation or brief hospitalisation days. There were also no reported long-term complications or deaths directly linked to the vaccination.”
“One of the known serious adverse effects is allergic reactions, which can lead to dizziness, shortness of breath, swelling of the face or throat, rashes, hives, or itching. The NPRA reported serious allergic reactions occurring in 1.5 cases per 1,000,000 doses. Another known serious adverse effect is myocarditis and pericarditis. These are inflammations of the heart muscles where patients can present with chest pains, difficult breathing, or heart palpitations. The NPRA reported 1.4 cases of myocarditis or pericarditis per 1,000,000 doses. However, most of these cases were mild in nature and the vaccine recipients responded well to treatment and recovered,” he explains further.
“Although the risk remains, it is important for people to understand that the benefits of taking the vaccine significantly outweighs the potentially harmful effects of the disease. In addition to this, many preventive steps are taken during the vaccination process to monitor and limit possible severe side effects from occurring,” he adds.
Lessons learnt from COVID-19 mass vaccination programme

Following many rigorous clinical trials and safety studies, a few of the COVID-19 vaccines were approved by the World Health Organization, followed by governmental approval from each country.
This marked the start of the global COVID-19 vaccination programme, which began with the distribution of these vaccines across the world. In Malaysia, COVID-19 vaccination centres were set up across the nation in an effort to vaccinate the population and achieve herd immunity.
Looking back, the global COVID-19 vaccination efforts have been a tremendous learning opportunity for everyone. From governments and healthcare institutions, all the way down to the average parents, there are many lessons we can take away from this.
Datuk Dr Zulkifli Ismail states, “Speaking on mRNA vaccinations as a whole, we have learnt that mRNA vaccines have plenty of advantages over traditional vaccines. Firstly, we have learnt that mRNA vaccines may be even safer when compared to a few of our traditional vaccines. Like the flu and HPV vaccines, the mRNA vaccines have no risk of infecting the individual being vaccinated, since no virus is involved unlike the Oral Polio Vaccine which uses a weakened poliovirus. In addition to this, the mRNA only stays in our body temporarily as it rapidly degrades in a few days.”
“However, the main advantage of the mRNA vaccines over traditional vaccines is the ability to boost its production and hence its availability. Traditional vaccines utilise a lot of resources to effectively produce a suitable antigen which can be used in a vaccine. However, mRNA technology instructs the human body to create the antigen which then stimulates the immune system to produce the protective antibodies. Thus, the manufacturing of mRNA vaccines can be readily enhanced, allowing for a more efficient vaccine production,” he further explains.
From a more local perspective, the COVID-19 vaccination programme has taught us many crucial lessons about how Malaysians view vaccinations. The chairman of Positive Parenting says, “We have also learnt many things about Malaysians’ attitude towards mRNA vaccinations. Studies have shown that acceptance of the COVID-19 vaccines amongst Malaysians is primarily influenced by its reported side effects, efficacy, and its status in a religious context, e.g. the halal status of the vaccine.”
“In addition to this, it was found that a driving factor behind vaccine hesitancy was distrust in the vaccine itself. This highlights the importance of reshaping the nation’s attitude towards COVID-19 vaccinations, particularly through educational campaigns that address these key areas,” he adds.
The future of mRNA vaccines: A bright or dark road?
The commercial introduction of the COVID-19 mRNA vaccine marks a historic achievement in modern medicine. In fact, the COVID-19 mRNA vaccine was only possible as it was built upon a foundation of decades of research.
As explained by Datuk Dr Zulkifli, “Many are unaware of this, but mRNA vaccine technology is not new. It has been used in clinical research for many years to study potential vaccines for Human Immunodeficiency Virus (HIV), Herpes Simplex Virus (HSV), Respiratory Syncytial Virus (RSV), Ebola Virus, and Zika Virus. Unfortunately, no promising mRNA vaccines for these diseases have been produced as of yet, primarily due to the lack of funding.”
Dato Dr Musa also adds, “Even though mRNA was first discovered in 1960, the first mRNA vaccines were only produced in 2020 at the onset of the COVID-19 pandemic. This was made possible with funding and investment by world health agencies and governments. It has spurred the development of other mRNA vaccines. There are at least 9 mRNA vaccines in the pipeline. The mRNA-HIV vaccine is now in Phase 1 clinical trials. Early results from the mRNA-RSV trial shows that the vaccine was 83.7% effective in reducing moderate RSV illness. There are also mRNA therapeutics against auto-immune disorders, cancers and inborn errors of metabolism, e.g. phenylketonuria and glycogen storage diseases.”
Dr Husna reminds us with a final remark, “Although the future for mRNA vaccines looks bright, turning that future into a reality begins with what we do today. To fulfil the promising future of mRNA vaccines, we have to collectively learn, understand, and accept mRNA technology as a society. This can start by fighting against vaccine misinformation. Whether it be through verified online sources, research papers, or through conversations with healthcare professionals, we should all strive to find accurate, correct, and scientifically backed information before making informed decisions on our health.”
Despite what many might think, the mRNA vaccines are not a new technology. The final common pathway is not novel. The mRNA instructs the body to make a (dead) sub-unit protein (spike protein) which elicits antibody production. This is not much different from the use of sub-unit proteins in Hepatitis B, HPV and inactivated flu vaccines. The novelty lies in using mRNA to enter the cytoplasm (not nucleus), which then sits on the ribosomes and makes spike proteins which leave the cells and elicit an immune response. As the saying goes “The science of today is the technology of tomorrow”, and the future may be very bright for mRNA vaccines.







Comments