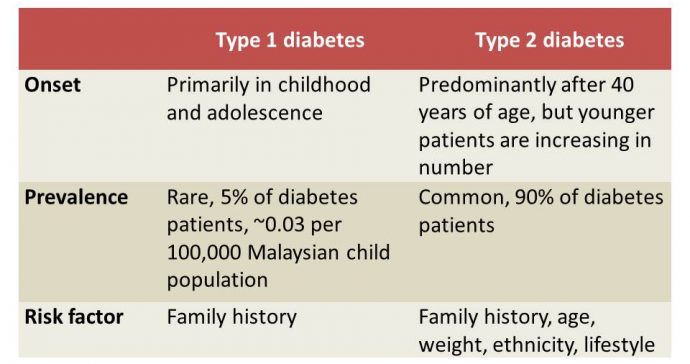
The mention of diabetes usually refers to type 2 diabetes (T2D), a worryingly common chronic illness among Malaysians. Type 1 diabetes (T1D) is lesser known, but the impact on life is equally serious.
T1D (previously known as juvenile or insulin-dependent diabetes) is a chronic condition whereby the pancreas starts to produce little or no insulin. Insulin is a hormone that helps control sugar levels in the blood and allows cells in the body to use sugar (glucose) from food for energy. The lack of insulin causes sugar to accumulate in the bloodstream, leading to the many diabetic symptoms and complications.
One possible cause of T1D is an autoimmune reaction that mistakenly destroys the insulin-producing beta cells in the pancreas. Exposure to certain triggers in the environment, such as a virus, is also linked to T1D. A major point that differentiates it from T2D is that T1D is not caused by lifestyle factors such as unhealthy eating habits or lack of physical activity.
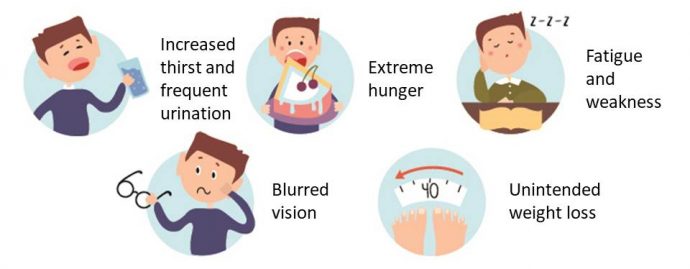
Common symptoms
T1D symptoms may appear suddenly, unlike T2D symptoms that develop gradually and are easily missed. Early diagnosis is important to avoid serious complications, such as diabetic ketoacidosis (DKA), but misdiagnosis as acute gastroenteritis or urinary tract infection can happen and should be avoided. T1D common symptoms are:
At the clinic, about 70% of local T1D cases show DKA symptoms, which include vomiting, abdominal pain, rapid breathing and loss of consciousness. DKA is life-threatening and must be treated as an emergency.
Acute complications
- Hypoglycaemia. Blood sugar level becomes too low due to high insulin level when a T1D child delays a meal/snack, does not eat enough or exercises too much. It happens quickly and needs immediate treatment. Symptoms include shaking, nausea, sweating and fatigue.
- DKA. The body breaks down fat cells when it cannot get enough glucose for fuel, resulting in chemicals called ketones. This happens when the child misses his insulin injections or during inappropriate management of sick-days. The combination of high glucose, dehydration and ketones build-up leads to ketoacidosis, which can be fatal.
Chronic complications
- Cardiovascular disease. The risk of cardiovascular problems, such as heart attack, stroke, atherosclerosis, high blood pressure and coronary artery disease, increases with diabetes.
- Organ damage. Blood vessels in organs like the eyes and kidneys can be damaged due to diabetes, causing kidney failure and serious eye conditions like cataract, glaucoma or blindness.
- Nerve damage. It starts with tingling, numbness or a burning sensation in the feet, and gradually spreads upward. Over time, it can lead to total loss of sensation, and even loss of limbs. Nerve damage also affects the gastrointestinal tract.
Management

- Insulin administration. A child with T1D needs lifelong insulin therapy to control his blood sugar. It can be administered via multiple daily injections or an insulin pump. There are short-acting, rapid-acting and long-acting insulin. Following a proper schedule for daily insulin administration is key to managing T1D.

- Blood sugar monitoring. Careful and regular monitoring of blood sugar level is important to ensure it remains within the target range. Check blood sugar level before and after eating, sleeping, exercising, driving or when low blood sugar is suspected. Self-monitoring with dextrostix (a test strip) is the standard way of measuring blood sugar, while intermittent and real-time continuous glucose monitoring systems are more advanced.

- Healthy eating. The child and his family need to understand how different food affects his blood sugar. Parents together with a dietician can propose a suitable diet plan focusing on whole grains, veggies and fruits. Insulin doses should be tailored to the amount of carbohydrate taken, so the child and his caretakers need to learn to count the carbohydrate content in his foods and drinks. There is NO specific diet restriction for T1D patients, but healthy eating is mandatory!
- Physical activity. Regular exercise is still necessary, but the child needs to know it lowers blood sugar. Thus, his blood sugar needs to be monitored more frequently when starting a new activity to observe any effect. His meal plan or insulin doses may need to be modified to suit the new activity.
Being diagnosed with T1D can be a huge challenge for a child and his family. Apart from the need for cautious management, T1D is also a costly disease – while insulin is free at government hospitals, other medications, equipment and overhead costs can strain family’s finances as diabetes is a long-term condition. However, T1D can be managed successfully. With the right help and support, especially from parents, family members and a good healthcare team, a T1D child can cope with his condition and live a regular, healthy life.
An educational contribution by Malaysian Paediatric Association.






Comments