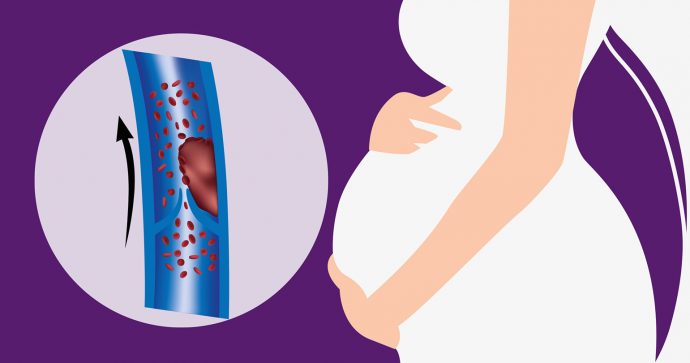
Venous thromboembolism (VTE) occurs when a blood clot forms in the vein, blocking blood flow in the area. Anyone can be inflicted with VTE, but some people are at a higher risk, including pregnant women.
According to the Department of Statistics, obstetric embolism, including VTE, remains the leading cause of maternal mortality in Malaysia. Between 1 in 500 and 1 in 2000 pregnancies are affected by VTE, more commonly during postpartum (six weeks after labour).
Percentage of maternal death in Malaysia due to obstetric embolism
2016: 23%
2017: 26%
Types of VTE
- Deep vein thrombosis (DVT) is a blood clot that forms in the deep vein, usually in the leg or pelvis, but can also develop in the arm. Symptoms include swelling, pain, warmth and redness of the skin, but 50% of cases show no symptoms. DVT is three times more common than pulmonary embolism during pregnancy.
- Pulmonary embolism (PE) happens when a DVT clot breaks off and travels to the lungs. It is potentially fatal and causes breathing difficulties, chest pains, rapid or irregular heartbeat, coughing up blood, dizziness or fainting.
Pregnancy increases the risk of VTE by four or five times due to blood hypercoagulability in pregnant women, a condition where blood clots more easily to minimise blood loss during childbirth. Other reasons include venous stasis (veins around the pelvis are compressed by the growing uterus) as well as blood vessel injury during delivery.
All pregnant women must be assessed for VTE risk factors in early pregnancy and after delivery. They will be categorised into high risk, intermediate risk or low risk groups, and advised to take appropriate preventive measures, including taking prescription prophylactic drugs, as well as asked to move around constantly and avoid dehydration.
Risk factors
Multiple factors increase VTE risk during pregnancy and postpartum. These include:
- Previous VTE
- Family history of VTE
- Age (higher risk as you age)
- Obesity
- Inherited clotting disorders
- Certain chronic diseases, e.g. heart/lung disease, cancer, inflammatory conditions, SLE, etc.
- Vein injury, e.g. due to major surgery, fractures or muscle injury
- Immobility, e.g. due to paralysis, prolonged confinement to bed, long- haul travel
- Increased oestrogen, e.g. due to birth control pills, hormone replacement therapy
- Caesarean section in labour
Treating VTE

Low molecular weight heparin (LMWH) is the recommended prophylactic and therapeutic medication for VTE in pregnancy. Other anticoagulants are less effective – e.g. unfiltered heparin (UFH) is linked with a higher risk of complications and fondaparinux is not recommended as it can cross the placenta. In severe cases, thrombolytic drugs can be used to dissolve the clot and surgery may be necessary for clot removal.
When diagnosed with VTE, LMWH treatment should be continued throughout pregnancy. However, it must stop once labour starts or 24 hours before planned delivery. Treatment should resume after delivery for six weeks, either with LMWH or warfarin (another type of medication). Both medications are safe for breastfeeding.
Compression stockings (special tight socks) may be recommended to help with blood flow and relieve pain and swelling. As a preventive measure, the sock should be worn on the affected leg for at least two years after having VTE. It also reduces the risk of post- thrombotic syndrome (PTS), a possible VTE complication that causes pain, discoloration, scaling or ulcers on the affected area, which can lead to disability.
This condition is one of the major risks that pregnant women have to face, and emphasises the need for optimal thromboprophylaxis (use of medication to prevent VTE) and treatment whenever indicated.
Local concerns
LMWH has been clinically proven as the most effective and safest anticoagulant treatment for pregnant women. However, the porcine origin of LMWH could be a concern among some Muslims in Malaysia. This may have affected the uptake of LMWH and is possibly one of the factors to the rising mortality rate of VTE.
Despite the origin, tests have shown that after extensive processes during production, no more porcine elements are traceable in LMWH. Many other Muslim countries have also allowed the use of LMWH due to its benefit and superiority to its alternative, especially for pregnant women. Muslim scholars agree that LMWH is allowed in a high risk VTE case as it can be regarded as a medical emergency and is required for life preservation.
An educational collaboration with Obstetrical and Gynaecological Society of Malaysia.






Comments