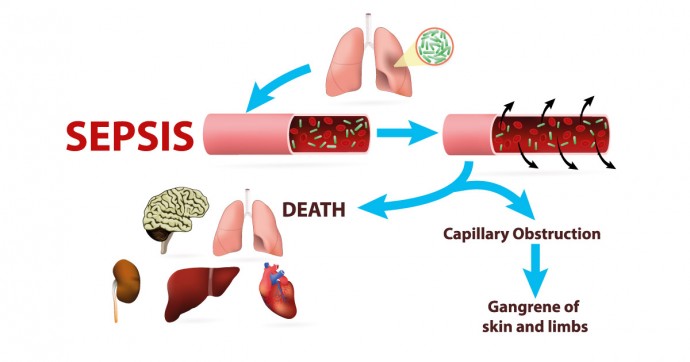
Meningococcal septicaemia, also called meningococcaemia (pronounced “man-ning-go-ko(h)-see-mia”, refers to a sudden onset of a bloodstream infection.
Complications include limb or hearing loss, cognitive dysfunction, visual impairment, learning difficulties, developmental delays, motor nerve deficits, seizure disorders, and possibly death.
Tiny but deadly
The bacteria Neisseria meningitidis is the culprit behind meningococcal septicaemia. It can also cause meningitis and pneumonia. It is endemic to the ‘meningitis belt’ of sub-Saharan Africa, and can easily live in the upper respiratory tract of healthy humans without causing illness. Anyone visiting these areas may become a carrier who unwittingly spreads the disease.
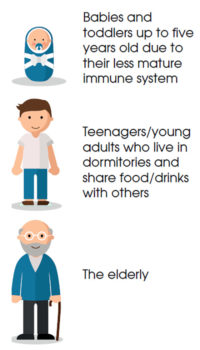
The National Institute of Health and Care Excellence (the Department of Health, United Kingdom) states that N. meningitidis causes bacterial meningitis in 1 out of 7 cases, or septicaemia in 1 of 4 cases, or as a combination in 3 out of 5 cases. In Malaysia, although bacterial sepsis accounts for almost 8% of newborn deaths (babies under-28 days), it should not be taken lightly. Meningococcal septicaemia (and meningitis) can cause death in hours.
Survivors have also been known to suffer from long term after-effects such as memory loss or difficulty retaining information, lack of concentration, clumsiness or problems with physical coordination, arthritis or joint stiffness, physical scarring of skin, possible loss of limbs (fingers, toes, arms or legs), and possible damage to lungs or kidneys.
Who are at risk?
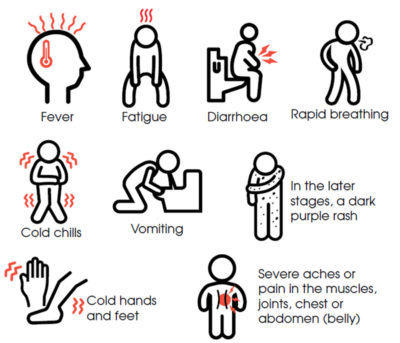
Signs/symptoms:
Be alert and don’t be afraid to seek immediate medical attention, if you suspect your child has meningococcaemia. The early signs/symptoms can be non-specific, thus making it difficult to distinguish from other less dangerous infections. However, if no attention is given to it, matters can quickly escalate (in as little as 24-48 hours), with more specific (and severe) signs and symptoms appearing over time.
The glass test
You can use the ‘glass test’ to check whether the rash is an indication of meningococcaemia or not. A regular rash will blanch (or fade) under pressure from a glass held against it. Purpuric rash of meningococcaemia will not blanch.
Don’t be a statistic
Early medical intervention can give your child a higher chance of survival. However, there is a very real risk of permanent physical consequences such as amputation of fingers, toes, arms or legs (due to a lack of blood circulation to these body parts), severe scarring due to skin grafts, and other mental effects such as loss of memory.
Prevention is the best cure, and meningococcaemia can be prevented by immunisation. Other steps you can take to minimise your child’s risk is by practising (and teaching him) good hygiene to reduce the spread of bacteria. Avoid sharing food or drink, and toothbrushes as well.
Speak with your paediatrician or doctor for options to protect yourself and your family from this deadly threat. Although it is not a common disease, its severity means that you should not be lax and assume that it will not happen to you. Take action by getting vaccinated.
An educational contribution by Malaysian Paediatric Association.






Comments