Your son has just been diagnosed with severe haemophilia. You feel devastated, frightened, sad and shocked. You seek advice from your doctor, read educational materials and connect with other parents. As you get better informed you feel empowered and find the strength to cope with this new journey.
What is Haemophilia?
Haemophilia is a life-long bleeding disorder caused by a defective factor VIII or IX gene on the X-chromosome, which interferes with the clotting process. It affects the male child. There may be a history of haemophilia on the mother’s side of the family but sometimes it can occur spontaneously.
Severity of Haemophilia
Haemophilia can be categorised into severe, moderate or mild according to the level of factor in the body. Severe haemophilia (factor level <1%) can cause spontaneous bleeding without any apparent trauma, while moderate (factor level 1 to 5%) and mild haemophilia (factor level >5%) will usually bleed following trauma.
Bleeding Manifestations
Bruises are common when the child starts to crawl but they do not usually require treatment. Gum bleeds commonly occur following trauma or teething. Get your child to suck on ice lollies to stop the bleeding. If bleeding persists, seek treatment at your haemophilia centre.
Haemarthrosis or bleeding into the joints is the hallmark of haemophilia. It usually occurs from year 1 onwards, when your child starts to walk. It commonly affects the knees, ankles and elbows and is extremely painful. Your child may not be able to move the affected limb.
Bleeding into muscles is another feature of haemophilia. Both joint and muscle bleeds have to be treated promptly and adequately, to prevent joint damage and muscle contractures.
Bleeding into the head, throat, neck, stomach and kidneys are serious and require urgent attention. The following are signs and symptoms that require you to contact your haemophilia team and seek immediate treatment:
- Your child receives a hard blow to the head
- He lacks alertness and seems drowsy
- He has episodes of vomiting
- He has seizures
- His neck is swollen and discoloured
- His cries sound different than usual
- He has trouble breathing
- His stools are bloody, black or tar-like
- He looks weak or pale
- He has back pain
- He has bright red or cola-coloured urine
If factors are available at home and you know how to access a vein, immediately infuse 50 IU/kg of factor to your child before heading to the hospital.
Haemophilia Team Members
The core team should consist of the following members:
- a medical director (preferably a paediatric and/or adult haematologist)
- a nurse coordinator who:
- coordinates the provision of care
- educates patients and their families
- acts as the first contact for patients with an acute problem or who require follow-up
- is able to assess patients and institute initial care where appropriate
- a pharmacist who ensures adherence to therapy and availability of factors
- a musculoskeletal expert (physiotherapist, occupational therapist, orthopaedic surgeon, rheumatologist) who can address prevention as well as treatment
- a laboratory specialist
- a psychosocial expert (preferably a social worker, or a psychologist) familiar with available community resources
Treatment
A child born with haemophilia today can lead a normal healthy life free from joint damage with prophylaxis i.e. regular factor infusions to prevent bleeding complications. This is usually started from 12 months of age. Parents are taught all about haemophilia and how to dose, access the vein and infuse the factor. Once they are confident, they bring the factors home and continue with home therapy.
Home therapy allows early treatment of bleeds by replacing the factor that is missing; factor VIII for haemophilia A and factor IX for haemophilia B. If in doubt or if the bleed is serious, treat first and then contact your haemophilia team.
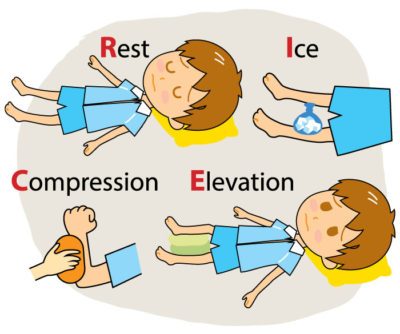
Besides factor replacement, apply RICE therapy – rest, ice, compression and elevation to the affected joint.
Once the bleeding and joint pain have subsided it is important to start exercises. Strong muscles protect the joints from further bleeds. This should be supervised by an experienced physiotherapist. Owning a pair of crutches is important to take the strain off the other joints, in the event of a joint bleed in the lower limb.
All bleeds and infusion of factors must be documented in a diary. This is important for monitoring treatment outcomes and factor usage.
Advice to parents
- It is normal to feel guilty about having a child with haemophilia, but you must remember it is neither parent’s fault.
- Don’t be overprotective – if you don’t allow your child to take reasonable risks he may not learn to become independent.
- Accept the fact that neither you nor your child can prevent all bleeds. You should not blame yourself or your child for bleeding episodes.
- Realize that the time your child spends crying during an infusion is a small price to pay for the long-term benefits of prophylaxis therapy.
- Help your son understand that haemophilia is just one aspect of his life and don’t allow him to use his haemophilia to avoid responsibilities or break rules.
- Encourage siblings to discuss haemophilia openly with you and their brother.
- Include siblings in the general care of the child and do not blame or punish siblings if the child bleeds.









Comments