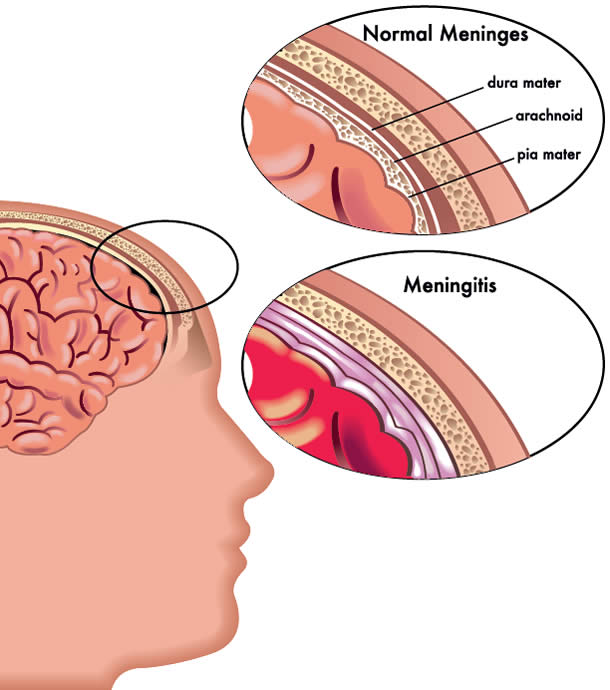
Meningitis is the inflammation of the protective membranes surrounding the brain and spinal cord called the meninges.
It can occur as a response to infection (bacteria, viruses, parasites, or fungi) or due to physical injury, cancer, or the body’s reaction to certain drugs. Although meningitis is not restricted to any one particular age group, children below two years of age face the highest risk. Some of the bacterial and viral meningitis can be prevented. Protecting them with early immunisation is the key to preventing the disastrous consequences of the disease.
Meningitis has been found to be much more common in developing countries. Environmental factors such as exposure to smoke, as well as medical conditions and immunodeficiencies can make one more susceptible to the disease.
Did you know?
According to the World Health Organisation (WHO), bacterial meningitis is responsible for an estimated 170,000 deaths worldwide. Death or disability can happen in as little as 24 hours from the first symptom. In the case of meningococcal meningitis, survivors can be left with serious medical problems including amputation of limbs/fingers/toes, severe scarring, brain damage, hearing loss, kidney damage, and psychological problems.
The types of meningitis These include bacterial meningitis, viral meningitis, parasitic meningitis, fungal meningitis and noninfectious meningitis.
- Bacterial meningitis: Bacterial meningitis can be a life-threatening infection, and is caused by bacteria such as Haemophilus influenza b (Hib), Neisseria meningitidis and Streptococcus pneumoniae. These organisms are not as contagious as the common cold or flu, but they can be spread through activities such as kissing, sharing of utensils/cups/cigarettes, close proximity (e.g. childcare centres), or activities in close quarters (e.g. colleges, universities, national service camps, dormitories).
- Viral meningitis: Viral meningitis is caused by enteroviruses, herpes simplex and varicellazoster virus (responsible for chicken pox and shingles). It can be spread through respiratory secretions or faecal contamination. It can affect any age group, but usually occurs in children below five years of age. It is serious, but rarely fatal in people with normal immune systems.
- Fungal and parasitic meningitis: Fungi and parasites that cause meningitis are quite rare. The most common fungal meningitis is caused by Cryptococcus. Parasitic meningitis is a very rare form of meningitis, but is often fatal. The parasite is an amoeba called Naegleria fowleri that can be found in bodies of warm freshwater (lakes or rivers) and poorly maintained swimming pools that are poorly or not chlorinated.
Other causes of non-infectious meningitis include cancers, lupus, certain drugs, head injury, and brain surgery. Immunisation
Signs and symptoms
The most common symptoms of meningitis in infants include fever, bulging fontanelle, nausea and vomiting, irritability (babies may cry when you pick them up), poor appetite, or drowsiness.
Older children may also have a sudden onset of fever or complain of headache or a stiff neck. Other symptoms include nausea, vomiting, sensitivity to light (photophobia), altered mental state (confusion or delirium). Meningococcal meningitis is often accompanied by the classic symptoms of a haemorrhagic purpuric rash (rashes that do not blanch on pressure).
While these are some of the more common symptoms, not everyone gets every symptom. Bear in mind that different kinds of meningitis may cause different symptoms. Hence, it is important to be alert and get immediate medical attention as quickly as possible.
Important!
If you suspect that you or someone in your family has symptoms and signs suggestive of meningitis, seek medical attention immediately. Early treatment of meningitis can prevent serious complications.
Determining the cause of meningitis
The best means to determine whether it is meningitis, and its specific cause, is by drawing samples of blood or cerebrospinal fluid (CSF) with a procedure called a lumbar puncture (LP). The LP procedure involves collecting CSF from the lower spine with a carefully inserted needle. The entire process will take less than half an hour.
A local anaesthetic is injected over the tail end of the back to prevent pain. A small spinal needle is then inserted into the lower back area, and your paediatrician will collect the CSF sample before withdrawing the needle. The CSF samples will be analysed and tested at a lab to find the specific cause of meningitis.
The results will help your child’s paediatrician to determine the most appropriate treatment for your child. In the case of bacterial meningitis, antibiotics can help prevent severe illness and reduce or stop the infection from spreading into the blood stream and from person-to-person.
To eliminate, vaccinate!
Some of the germs which cause meningitis and can be prevented by immunisation are tuberculosis, polio, Hib, measles, mumps, chicken pox, pneumococcus and meningococcus.
Meningococcal meningitis can now be prevented with the Meningococcal Conjugate Vaccine (MCV) which is now available in Malaysia. Four strains of Neisseria meningitides, (A, C, W, and Y) can be protected with the quadrivalent MCV4.
Recommended by WHO
WHO recommends MCV4 for infants at two doses between the age of nine and 23 months (with at least three months interval between doses), and one dose for children older than two years. The Centers for Disease Control and Prevention (CDC) advocates vaccinating preteens and teens at age 11, with a booster dose by 18 years of age.
MCV4 vaccines have been shown to be safe and efficacious in children aged nine months and older. They are far superior to the older generation of Meningococcal Polysaccharide Vaccine (MPV4) as they provide a longer period of protection and can be used in younger children below 2 years old who are highest at risk. Currently, vaccination against other more common causes of meningitis, which include Hib, measles and mumps are included as part of the Malaysian National Immunisation Programme. Unfortunately, MCV4 is not included.
Maintaining good personal hygiene may lower your chances of getting infected or spreading the disease to others. However, the best option is still to make sure that you and your child are vaccinated. Don’t wait for a tragedy to happen. Ask your child’s paediatrician or doctor about meningitis prevention or call your health-care provider to schedule a vaccination appointment.







Comments