During pregnancy, you and baby are intimately linked and your respective health status and well-being are intertwined. For this reason, you will need to attend a succession of antenatal check-ups, starting in the first trimester, before the 12th week, to enable the doctor to monitor your condition and baby’s progress.
Like most mothers, you might be confused by the variety of tests to which you will be subjected.You might even become anxious should the doctor order certain special, non-routine tests. Here is an explanation of antenatal check-ups and the tests they involve to help you better appreciate their importance.
Checking on Mom
Your first antenatal check-up.
The doctor will go over your medical history, giving particular attention to your current health and lifestyle. You will also receive a physical examination that covers your blood pressure, heart, lungs, thyroid, breasts, and teeth. Similarly, you will take blood tests to check for possible anaemia and your status with regard to various diseases (eg rubella immunisation status, and hepatitis B and HIV carrier status).
Subsequent routine check-ups.
Unless you have a health or pregnancy problem (which may necessitate more frequent checkups), you will generally visit the doctor once a month until week 28, every fortnight after week 28 to week 36, and weekly from week 36 until delivery.
At each visit, the doctor will weigh you as well as take your blood pressure and analyse your urine. These procedures will help her look out for warning signs of preeclampsia – a combination of high blood pressure, fluid retention and protein in the urine. Also known as pre-eclamptic toxaemia, this condition affects 1 or 2 out of every 20 mothers, especially in the second half of their pregnancy. Mild preeclampsia is usually easy to treat but, if uncontrolled, it could lead to eclampsia and bring on seizures and coma.
Your urine sample will also be checked for the presence of infections and indications of gestational diabetes. This type of diabetes is induced by pregnancy and needs to be confirmed by a further test. Medication and careful dietary changes may be necessary to help bring high blood sugar under control. At 22 weeks or later, the doctor may vaccinate you against tetanus to prevent tetanus in your baby after birth. If this is your first pregnancy, the injection will be repeated a month later.
Checking on Baby
By feeling.
By palpating (using the fingertips to press) your abdomen, the doctor will be able to locate the top of your uterus to assess the foetus’ growth rate. From week 34 or 36, the doctor may also request that you monitor your baby’s movements. If baby’s oxygen supply is sufficient, he should move about at least 10 times over 12 hours. Baby may be more sluggish if he has a twin or a mother who smokes, has diabetes or high blood pressure.
By listening.
After week 14, the doctor will listen for baby’s heartbeat using either an electronic sonicaid or, after week 22, a trumpet-like foetal stethoscope. In the last 2 months of pregnancy and, if necessary, the doctor may perform a cardiotocography test which measures baby’s heart rate with an electronic monitor. Abnormal sounds, rhythms and heart rates may indicate a compromised baby.
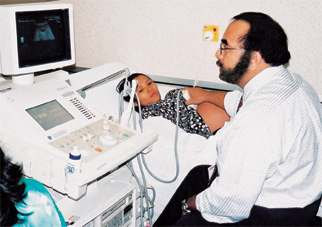
By scanning.
From very early in pregnancy, an ultrasound scan may be performed. Seeing the foetus’ image on an electronic screen may help reassure you that baby is doing well. However, more regular ultrasound scans may be necessary if you have had a previous miscarriage or are experiencing pain or bleeding. The same applies if the doctor thinks that the foetus is not growing properly.
Special tests for chromosomal abnormalities.
If you are over 35 of age or carry the risk of passing on certain birth defects or genetic diseases, the doctor may advise you to undergo some of the special tests below.
- Blood tests. The Triple Test at weeks 14-16 measures three blood chemicals (AFP, estriol and the pregnancy hormone called hCG) to detect the possibility of neural tube defects (eg spina bifida) and syndromes such as Down.
- Scans. The Nuchal Translucency Scan, using ultrasound, measures fluid accumulation at the back of baby’s neck. Conducted at weeks 10-12, it is used to detect possible signs of Down syndrome (a chromosomal disorder affecting development) and Turner syndrome (a chromosomal disorder affecting growth and sexual development in female babies).
- Invasive tests. Amniocentesis, which can be done any time beyond week 13, is where a needle is inserted through your abdomen to draw a sample of the fluid inside the uterus. The fluid is used to detect Down syndrome, and other chromosomal abnormalities. Another invasive test is Chorionic Villus Sampling which can be performed towards the end of the first trimester or later. It entails using a needle to extract miniscule tissue samples from the placenta to check for Down syndrome and blood disorders, such as thalassaemia major. These invasive tests are particularly important if the baby is suspected of chromosomal or certain genetic problems.
Like any other mother, you would dearly wish for a normal, healthy child. Thus, you would do well by being receptive to good antenatal care and the tests that may come your way. No test is perfect and the findings may not always be accurate. However, it always helps to know how you and your unborn child are doing. The information will put you in better stead to care for the both of you, and to ensure early intervention if either is in trouble.







Comments