Allergies happen when our immune system overreacts to allergens, which are foreign substances that are not normally harmful. Over the last few decades, allergic diseases have been on the rise.
Allergies can affect a person differently, depending on factors such as the type of allergy and how sensitive that person is to the allergens. Some examples of allergies include drugs, foods, or even pet fur. Cow’s milk protein allergy (CMPA) is fairly common and it is estimated to affect up to 8% of children globally.
How allergies develop
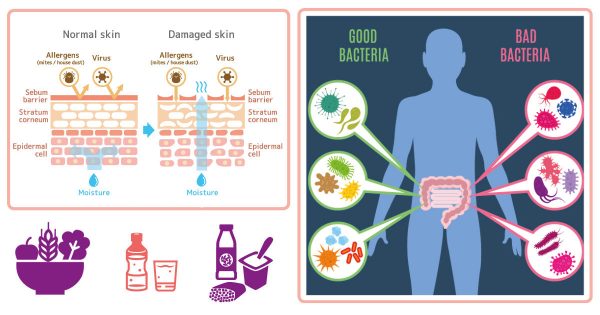
Multiple factors form the basis for the development of allergies. Most importantly, the immune system has to learn how to respond appropriately to foreign substances, and it has been found that sufficient early exposure to a variety of different stimuli often leads to a better response.
This process helps to ‘train’ your child’s immune system to react optimally, and to better recognise a harmless substance without treating it like an invader. While this ‘training’ can be easily done with adequate exposure to the environment, the immune system needs to be strengthened too, this begins from the gut.
A good start is important
The gut, which is also home to trillions of microorganisms that are collectively known as gut microbiota, is closely linked to gut health and the immune system. Formed early in life, the initial ‘seeding’ comes from vaginal delivery and subsequent breastfeeding. Other factors of gut microbiota development include maternal and infant diet, pollutants in the environment, and antibiotic use.
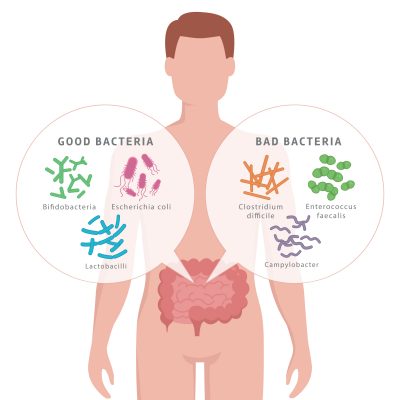
A healthy gut microbiota contains a balance of 85% good bacteria vs 15% bad bacteria. The imbalance of our gut microbiota is called gut dysbiosis. Emerging
researches point to this as a potential cause or trigger for the development of allergic diseases. The gut microbiota actually helps regulate how our body responds to the antigens that cause allergic responses, hence the importance to reduce the occurrence of dysbiosis.
What causes dysbiosis
There are several possible factors of dysbiosis:
- Sudden dietary changes, e.g. excessive consumption of sugar or refined starch.
- Accidental consumption of chemicals, e.g. pesticides on fruit/veggie or excessive use of household cleaner that leaves a residue.
- Medications, especially antibiotics, which can also kill good bacteria. If your child is ill, do not demand for antibiotics if your doctor does not prescribe any. Antibiotics do not work on viral illnesses but has been shown to affect gut microbiota composition as it kills both good and bad bacteria. Inform your doctor if you are breastfeeding and find out whether the medication is safe for use and its side effects。
Lowering the risk of dysbiosis
You can minimise the risk of gut dysbiosis in your child by practising exclusive breastfeeding for the first six months, followed by complementary feeding at 6 months (and continue to breastfeed until 2 years old). Breast milk also contains good bacteria from the mother to colonise and help flourish the baby’s gut microbiota.
As your child grows older, serve healthy food (more veggies and fruits) with healthier cooking methods (less sugar, oil and salt). To maintain a balanced gut microbiota, his diet should also include probiotic-rich food (e.g. yoghurt, fermented food) or food products with added probiotics. Probiotics also need prebiotics, which are food for probiotics, found in certain non-digestible dietary fibres to stimulate growth of good bacteria. These include banana, onion, asparagus, and garlic.
Keeping your child’s gut health in tip-top order is crucial as more than 80% of the immune system lies in the gut and it is linked to allergies. Lastly, remember that while probiotics hold great promise for managing or treating allergies, one should not rely solely on probiotics; start introducing your child to a healthy lifestyle, coupled with regular physical activities from an early age, as this improves his chances of growing up healthy and strong.





Comments