As the number of COVID-19 victims continues to rise and the race against time to find its vaccine intensifies, one of the terms that has been hotly discussed is “herd immunity”. Let’s find out more about it.
Vaccination directly protects individuals who are vaccinated against certain infections, but it can also provide indirect protection to the unvaccinated in a population. This is what we call herd immunity or community immunity, a key aspect of epidemic control.
Recently, there have been calls from certain parties to let the pandemic run its course until the population can naturally achieve the so-called “herd immunity”. We need to understand and realise this proposal is a grave misinterpretation of the concept.
The right concept
To understand herd immunity, we need to be familiar with certain terms. Firstly, we have to know the infectiousness of a disease, indicated by its basic reproduction number (R0 or R-naught). It can be defined as the expected number of new infections generated by one infectious individual in a fully vulnerable population without any control measures.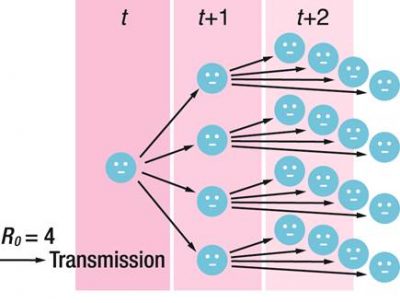 For example, an infectious disease with R0 = 4 means that 1 case is expected to generate 4 other cases. The higher the R0, the more infectious the disease is. R0 is unique to different diseases and may vary across populations and over time, depending on various factors.
For example, an infectious disease with R0 = 4 means that 1 case is expected to generate 4 other cases. The higher the R0, the more infectious the disease is. R0 is unique to different diseases and may vary across populations and over time, depending on various factors.
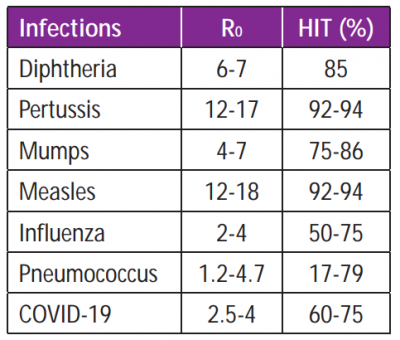
R0 determines the herd immunity threshold (HIT), which is the minimum level of vaccination coverage or immune individuals in a population that must be achieved to produce herd immunity against a certain infection. An easy way to calculate HIT is using this equation: HIT = 1 – 1/R0.
Hence, to achieve herd immunity against a disease with R0 = 4, at least 3/4 or 75% of the population have to be immunised. This calculation assumes that susceptible and infectious individuals in a population are equally in contact with one another and spread the infection in the same way.
Examples of infectious diseases with estimated R0 and HIT
From this, we can deduce that the more infectious the disease, the higher the R0, thus the higher the HIT and the more people that need to be vaccinated to achieve herd immunity in a population.
Optimal benefits
Various other factors play crucial roles to ensure that optimal herd immunity can be achieved via vaccination.
- High vaccine effectiveness. This is key to attain optimal herd immunity. Vaccine effectiveness varies between different populations and regions. However, not all vaccines stimulate lifelong immunity and this may decrease herd immunity. The effect of waning immunity can be mitigated by increasing vaccination coverage or taking booster shots.
- Reduced transmission potential (or force of infection) with vaccination. Vaccination needs to target the main reservoir of infection, i.e. groups who are most likely to get and spread infection. Low vaccine coverage among these groups may compromise herd immunity, even though overall coverage is high. This also depends on the route of transmission of the pathogen.
- Appropriate vaccine uptake (coverage, distribution, timing). Optimal herd immunity is more likely to be achieved when vaccine coverage is at the higher end of HIT. Another important factor is appropriate distribution patterns by targeting highly exposed (e.g. healthcare workers) and vulnerable (e.g. infants, elderly) populations. The timeliness in receiving the vaccine also impacts the effectiveness of the vaccination programme, and thus, the herd immunity.
A success story!
In the United Kingdom, the incidence of vaccine-type invasive pneumococcal disease (IPD) in unvaccinated elderly over 65 years old has been reduced by 81% after pneumococcal conjugate vaccine (PCV) was included as part of routine immunisation for infants under 2 years old. Hopefully, the pneumococcal vaccination programme in Malaysia that begins this December will be as successful.
Importance of herd immunity
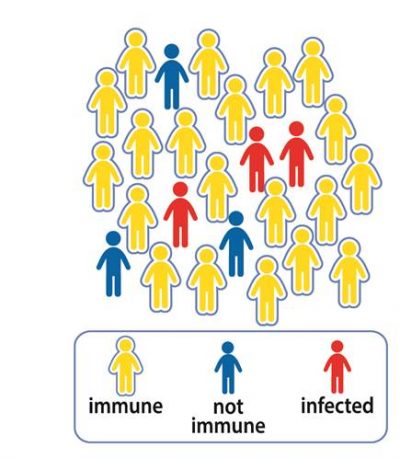
The best case scenario is to have 100% vaccine effectiveness and coverage, but the reality is far from perfect. No vaccine is 100% effective and there are people who cannot get vaccinated or do not elicit strong immune responses from vaccines.
These include newborns, people allergic to certain vaccines, people with weakened or failing immune systems, or elderly with chronic diseases. This is where herd immunity comes into play, providing indirect protection to these groups.
Optimal herd immunity via vaccination also counteracts waning immunity. Protection with certain vaccines can diminish with time, e.g. pertussis vaccination starts to weaken after 2 years. Thus, people with waning immunity are exposed to infection unless herd immunity is strong and vaccine uptake is sustained.
Who else should be vaccinated?
Apart from the vulnerable population, these groups of people should also get vaccinated.
- Families and close contacts of vulnerable population
- Caregivers of children, elderly and sick patients
- Healthcare/hospital workers
When you get yourself vaccinated, you’re not only protecting yourself, but also your loved ones and other vulnerable individuals in the population. As you can see now, vaccination is crucial and the safest way to achieve optimal herd immunity!
An educational contribution by Malaysian Paediatric Association.







Comments