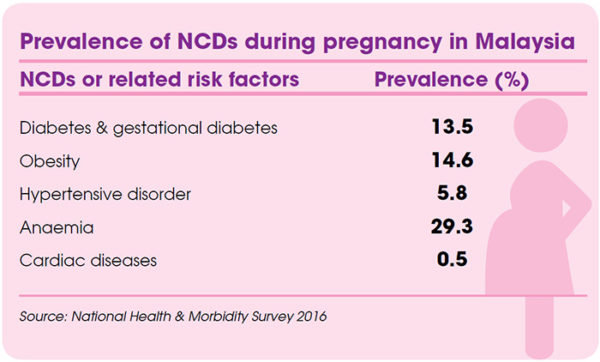
According to the World Health Organization (WHO), global maternal mortality decreased by 44% from 1990 to 2015. Most improvements have been focused on the most common and direct causes of maternal death, which include obstetric complications like abortion or obstructed delivery. However, indirect causes like non-communicable diseases (NCDs) and related risk factors were given lesser attention. In fact, almost 15% of maternal deaths were caused by pre-existing medical conditions including NCDs, according to a WHO analysis in 2014.
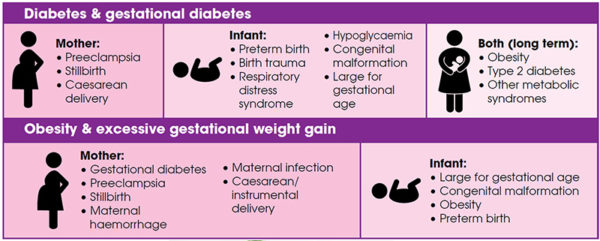
NCDs, also referred to as chronic diseases, develop over a long time and are caused by a combination of genetic, physiological, environmental, and behavioural factors. NCDs like diabetes, anaemia, and heart diseases can have serious and fatal effects on pregnancy. Metabolic risk factors for NCDs like obesity, high blood glucose, and hypertension can also lead to complications in both mother and baby. Pregnant women with NCDs have to properly manage their conditions to ensure safe delivery.
Possible complications
Cardiovascular concerns
Other NCDs also lead to various related complications during pregnancy. In fact, cardiac disease is the leading cause of maternal mortality during pregnancy in many developed countries. Women with pre-existing heart disease are exposed to both obstetric and cardiac complications if they become pregnant, and may be advised against pregnancy. Meanwhile, high blood pressure during pregnancy poses various risks such as decreased blood flow to the placenta, placental abruption, intrauterine growth restriction, and future cardiovascular disease in the mother. Mild anaemia is common in pregnancy, but if severe or untreated, can lead to complications like preterm birth, low-weight baby, postpartum depression, and offspring with anaemia.
Keeping a close watch
It is clear that pregnancy with NCDs is a serious health risk to mothers and their babies. Proper management of NCDs as well as preventive measures are important during pregnancy. Women with NCDs have to undergo preconception counselling with their obstetrician when planning for pregnancy to understand the risks. If they are getting pregnant, proper and timely antenatal and postpartum care is vital to keep track of their health status. In addition, universal screening for NCDs in pregnant women should be recommended as many are unaware that they suffer from NCDs. This is necessary for early detection and management of NCDs.
Medications may be prescribed to pregnant women with NCDs. For example, anaemia is usually caused by a low level of iron, folate, or vitamin B12 in blood, and can be treated by taking supplements or foods rich with these micronutrients. Other than that, treatment with insulin therapy or oral antidiabetic agents is vital for diabetic pregnant women. Women with pre-existing NCDs may be advised by doctors to change their medications when getting pregnant as some drugs can be harmful to the baby. Weight gain during pregnancy should also be monitored especially in obese or underweight mothers.
Of course, the ideal management for NCDs is prevention; it is never too late to start practising a healthy diet together with a physically activelifestyle. Nevertheless, there is a changing trend in maternal morbidity and mortality as more women of reproductive age are being affected by NCDs. The approach in maternal healthcare has to be realigned to address this concern.
An educational collaboration with Obstetrical and Gynaecological Society of Malaysia.






Comments