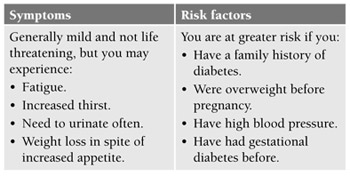
Gestational diabetes is a form of diabetes that develops during pregnancy, affecting up to 3% of pregnant women. You may develop the condition even if you never had diabetes before. It typically sets in during the second trimester, and resolves after baby is born. While sweet foods do not directly cause the condition, mums-to-be should pay extra care of their diet and activity level to reduce their risk of getting it.
The cause
Gestational diabetes is essentially the result of changing hormones during pregnancy. Some of the pregnancy hormones block the regular action of insulin, a hormone responsible for regulating blood sugar levels in the body. Insulin transforms excess sugar in the blood into glycogen, to be stored in the liver for later use. By blocking the action of insulin, the mother’s body ensures baby receives from the mother enough sugar, one of baby’s food sources while in the womb.
However, when insulin action is blocked, this also means the mother’s body is not able to utilise blood sugar efficiently. As a result, more insulin is needed to cope with the changes. If her body cannot produce enough insulin to meet this additional demand, it could lead to poorly controlled blood sugar levels, hence the diabetes.
How does it affect the baby?
When mum has diabetes, a high amount of sugar is transported from her blood stream through the placenta to the baby. While baby in the womb is able to produce insulin to use sugar, excessive sugar can have undesirable effects if the condition is not treated promptly.
Large baby (Macrosomia) – Baby produces more insulin that converts extra sugar into body fat, causing baby to grow larger than usual. This could pose difficulties during delivery, eg labour may be slowed down, baby is too large for vaginal delivery, increased risk of injury to baby during labour, and mum has a greater chance for a caesarean section.
Neonatal hypoglycaemia (low blood sugar) – Baby continues to produce large amounts of insulin for some time after delivery. Since maternal sugar supply is no longer present, the excess insulin will act on baby’s own reserves of blood sugar, causing hypoglycaemia in the newborn. Baby can become jittery or may even have breathing problems. This can be quickly corrected once baby receives breast milk or supplemental sugar water.
Other complications – Baby may have jaundice at birth. There is also a slightly higher chance of premature labour. While baby will not be born with diabetes, there is an increased risk of baby becoming obese or developing diabetes during childhood.
Treatments
Your doctor will check your blood sugar levels during your prenatal visits. If you are diagnosed with gestational diabetes, your doctor may recommend a diet plan. If necessary, you may be given medication for blood sugar control. Your doctor will keep monitoring both you and your baby throughout your pregnancy.
Reduce your risk
- If you are overweight, reduce weight to a normal range before you get pregnant to lower your risk of gestational diabetes.
- During your pregnancy, eat healthy and well-balanced meals.
- If you crave for something sweet, go for foods that contain natural sugars, such as fruit. Avoid foods high in simple sugar, eg ice-cream, cakes or cookies.
- Exercise daily to keep your blood sugar within safe levels. Ask your doctor to recommend activities that are suitable and safe for you.





Comments