WHILE eczema (dermatitis) can be a difficult disease, it is also a manageable one. With proper treatment and care, people with eczema can lead fulfilling lives and participate fully in school, work and family activities.
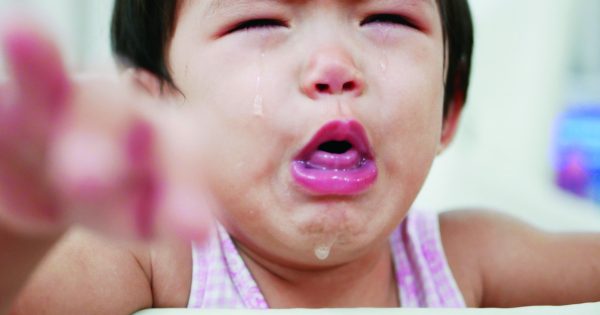
Eczema is an inflammation of the skin that flares up from time to time. Atopic dermatitis is the most common type of eczema, and usually strikes in early childhood before the age of five.
In eczema patients, moisture is easily lost from the skin, causing it to dry out and flake. Symptoms include: red to brownish-gray patches, itching, tiny raised bumps and vesicles that may leak fluid and crust over and thickened or scaly skin. Proper skin care and management of inflammation can usually ease the symptoms and keep the skin condition under control.
Moisturize, moisturize
Good skin care is essential in controlling eczema. For people with mild eczema, keeping their skin soft and moisturized by frequent and generous use of emollients may be all that is needed to improve and manage symptoms.
Emollients are non-cosmetic moisturisers that come in the form of creams, ointments and lotions. They keep skin moist and help prevent cracks, making it more comfortable and less itchy for eczema patients.
The type of emollient you should use would depend on the condition of your eczema, part of body skin that is involved and how you react to a specific ingredient or ingredients in an emollient.
Creams contain a mixture of water in fat, and have a light and cool effect on the skin. Due to this, many people with eczema prefer creams for daytime usage. However, creams may contain preservatives and might cause sensitivity, although such occurrences are rare.
Ointments do not contain preservatives, but they can be very greasy and may be cosmetically unappealing to some. However, they are very effective at retaining moisture in the skin, and are useful for very dry and thickened skin.
Lotions contain more water and less fat than creams but evaporate quickly and are not the most effective means to keep skin moisturised. However, they are easy to apply specially over hairy regions of the body.
Regular used of emollients may be all that you need in keeping mild eczema symptoms in check. However, people with more severe eczema may require medications to help control their flare-ups.

Medications for eczema control
Corticosteroid creams or ointments. Prescription corticosteroid creams or ointments can ease inflammation and relieve itching. Some low-potency corticosteroid creams are available over-the-counter, but you should always consult your doctor before using any topical corticosteroid. They are very effective and safe if used correctly.
Despite this, many people are concerned about potential side effects from topical steroids. The trick is to use the correct strength of steroid for the severity of the eczema and be prepared to change treatment as the severity of the eczema changes.
Topical steroids are usually discontinued when the symptoms disappear and are resumed when new patches arise. Topical steroids are safe if used correctly. Side effects of long-term topical corticosteroid use include skin irritation or discoloration, thinning of the skin, infections and stretch marks.
Antibiotics. You may require antibiotics if you have super added bacterial skin infection and the signs of bacterial infection include weeping, crusting, pustules or painful swelling. Your doctor may recommend taking a short course of antibiotics to treat an infection or sometimes hospital admission is necessary for intravenous treatment.
Oral antihistamines. Oral antihistamines may help with severe itching. However, antihistamines like Diphenhydramine (Benadryl, others) can make you sleepy. If your skin cracks open, your doctor may prescribe mildly astringent wet dressings to prevent infection.
Corticosteroids. For more severe eczema cases, your doctor may prescribe oral corticosteroids, such as prednisone, to reduce inflammation and to manage symptoms. These medications are effective, but often used in the short term only. They cannot be continued for more than a few weeks at a time without significant side effects.
Managing lifestyle factors
Flare-ups may be associated with lifestyle factors such as stress, physical activity, contact allergy and temperature changes.
Stress management is vital in controlling eczema. Often, it involves making time for rest and relaxation, and changing the reaction if the situation is unavoidable. Getting adequate sleep is also an important factor.
Also try to avoid known allergens such as dust mites, pollen, animal dander, and clothing materials like wool and synthetics. Food allergy affect a third of children with eczema and can cause flare-ups especially in children less than 2 years old. The common food which could flare eczema includes milk, eggs, and wheat, soy and peanut products.
People do develop flare-ups when they experience a sudden change in temperature. So where possible, try to anticipate changes in weather, especially when you travel into another country and arm yourself with effective treatments.
Lastly, try to avoid hot baths and don’t scratch if you develop itchy rashes. Few ways to control your itchy eczema are by rubbing, applying emollient, or apply a bag of ice to the affected areas and gently pinching the skin around the eczema to divert the itch sensation. It may also be helpful to keep your fingernails short to prevent injuries from scratching. Seek advice from your doctor if you have any doubts.






Comments